Understanding Pulmonary Compliance: Unraveling the Mechanics of Lung Function for Respiratory Therapy Students
- Jose Vazquez
- Oct 28, 2024
- 3 min read
Updated: Nov 7, 2024
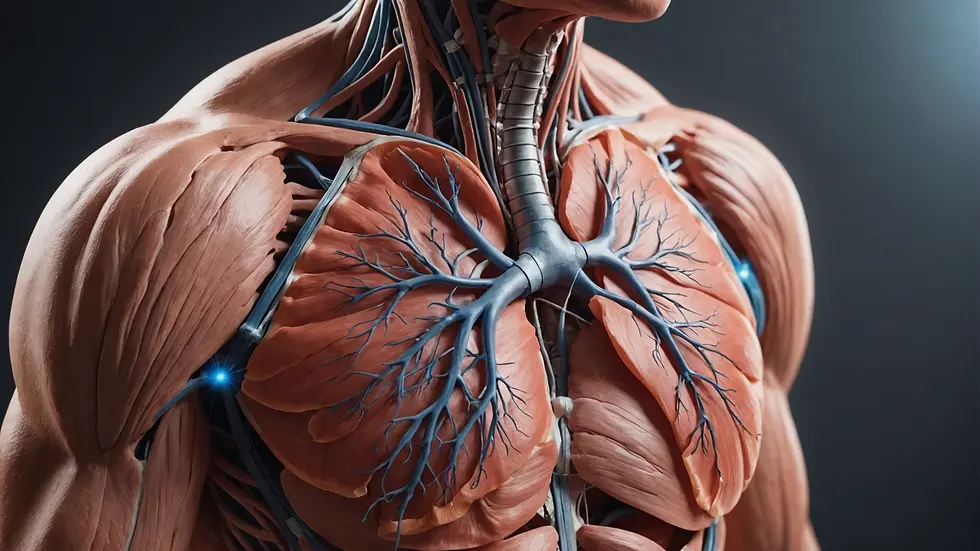
Pulmonary compliance is crucial for grasping lung function and mechanics. For respiratory therapy students, understanding this concept is vital for quality patient care, especially in conditions that impact breathing. This article will break down pulmonary compliance, its significance, and the various factors that affect it, enriching your knowledge for real-world applications.
What is Pulmonary Compliance?
Pulmonary compliance measures how easily the lungs stretch and expand when pressure changes. It quantifies the change in lung volume for a unit change in pressure. Simply put, it indicates how easily the lungs can inflate.
High Compliance: Indicates that the lungs expand easily, facilitating effective ventilation.
Low Compliance: Implies stiff, less flexible lungs that require more effort to expand, often leading to respiratory distress.
For example, normal lung compliance is about 0.1 to 0.2 L/cm H2O in adult patients, while patients with conditions like pulmonary fibrosis may experience compliance values significantly lower than this.

The Importance of Pulmonary Compliance in Respiratory Therapy
Understanding pulmonary compliance holds great value for respiratory therapy students for several reasons.
Patient Assessment: Monitoring lung compliance can help identify key conditions. For instance, patients with emphysema may show increased compliance values, whereas those with acute respiratory distress syndrome (ARDS) typically exhibit decreased compliance.
Ventilation Management: During mechanical ventilation, therapists must adjust settings based on a patient’s compliance to ensure adequate oxygenation. For example, in patients experiencing low compliance, clinicians might lower tidal volumes to avoid lung injury.
Therapeutic Approaches: Treatments like positive pressure ventilation and incentive spirometry can be customized based on a patient's compliance status. Tailored approaches can lead to better recovery outcomes for those requiring respiratory interventions.
By understanding how to evaluate and respond to pulmonary compliance, respiratory therapists can greatly enhance patient care.
Factors Affecting Pulmonary Compliance
Numerous factors can influence lung compliance, essential for accurately assessing patients with respiratory issues.
Age and Gender
Lung compliance changes with age. Older adults typically experience decreased compliance due to loss of elastic lung tissue. Research shows that adults aged 65 and older can have 30-50% lower compliance compared to their younger counterparts. Moreover, women generally have lower compliance than men, often due to smaller lung volumes.
Lung Pathologies
Lung diseases significantly alter compliance. Specific examples include:
Emphysema: This condition increases lung compliance due to the destruction of elastic tissue, often visualized as “floppy” lungs, making air trapping a common issue.
Pulmonary Fibrosis: Characterized by scarring and stiffening, this disease results in reduced compliance, making it hard for lungs to expand effectively.
Body Position
Positioning affects lung compliance. Studies show that patients lying flat may see a 25-30% decrease in lung volume and compliance compared to those sitting upright due to increased abdominal pressure. Changing a patient’s position can enhance lung volumes and improve overall compliance.
Respiratory Muscle Strength
Weakened respiratory muscles can lead to reduced lung expansion and decreased compliance. For example, in patients with conditions such as amyotrophic lateral sclerosis (ALS), the impairment of respiratory muscle function greatly affects lung compliance.
Physiological Factors
Conditions such as obesity and pregnancy can greatly impact pulmonary compliance. For instance, obesity can lead to up to a 50% reduction in functional residual capacity (FRC) due to increased pressure on the diaphragm. Similarly, during pregnancy, the growing uterus alters the diaphragm's position, potentially limiting lung expansion.
Measuring Pulmonary Compliance
Pulmonary compliance can be measured in various ways:
Static Compliance Measurement: Calculated by dividing the volume of air delivered to the lungs by the change in pressure during mechanical ventilation.
Dynamic Compliance Measurement: Assessed during the breathing process and considers airway resistance, providing a more accurate picture of lung behavior.
To interpret these measurements effectively, respiratory therapy students must grasp the clinical implications of compliance values in patient care.
Clinical Implications of Pulmonary Compliance
Understanding pulmonary compliance not only helps with patient assessment and treatment but also significantly influences outcomes in critical care.
For instance, in ARDS patients, recognizing compliance status helps determine optimal tidal volumes. It is crucial to maintain tidal volumes between 4-6 mL/kg to avoid additional lung injury. Early detection of changes in compliance allows teams to implement targeted interventions, ultimately enhancing patient recovery and minimizing complications.
Key Takeaways for Your Future Practice
Pulmonary compliance is a foundational aspect of lung function crucial for respiratory therapy. Recognizing its role in patient assessment, treatment strategies, and outcomes will significantly enhance care for your patients.
By mastering factors influencing compliance and measurement techniques, you will be well-positioned for success in respiratory care. Make pulmonary compliance a key focus in your studies and practice, preparing you for the challenges of your future career as a proficient respiratory therapist.




Comments